Sanya Dhingra

New Delhi: The Narendra Modi government plans to roll out a ‘One Nation, One Health System’ policy by 2030, which would integrate modern and traditional systems of medicine like allopathy, homoeopathy and Ayurveda in medical practice, education and research.
Government sources told ThePrint that the policy aims to formulate an Integrative Health System, under which patients would get treatment from any medicinal system, depending on what ails them and their current condition.
“There is a need to integrate the different forms of treatment. The government is trying to shift the focus away from the ‘-pathy’ part of medicine, which means that it should not matter if it is allopathy, homoeopathy or Ayurveda, as long as the person benefits from the treatment,” a government official said on the condition of anonymity.
“If a patient comes to a hospital, they can be given allopathic treatment if their condition is serious, but they can also be given homoeopathic or Ayurvedic treatment in the same hospital if their condition can be managed with those,” the official explained.
He added that the scheme would be recognition of the fact that in India, there are traditional forms of medicine that are not “alternative” but very integral to healthcare.
When reached for a comment on this, the Union Ministry of Health & Family Welfare spokesperson told ThePrint “this is an initiative of NITI Aayog” and the query should be directed to the government’s planning think-tank.
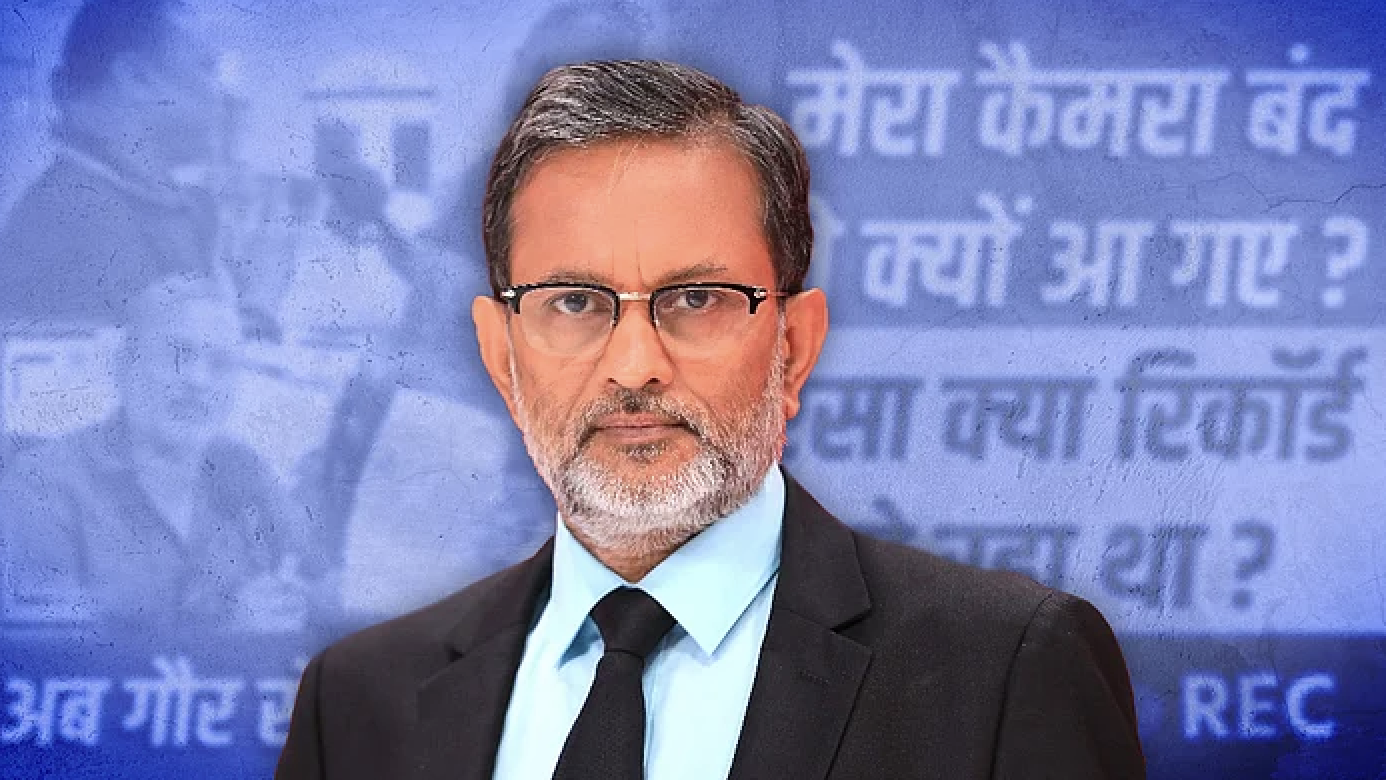
ThePrint tried to contact Dr V.K. Paul, member (health) of NITI Aayog, via text message and call for a comment, but he did not reply. This report will be updated when a response is received.
Re-envisioning medicine in Indian context
A meeting chaired by Dr Paul was held on 8 September to begin formulating the new system.
According to the minutes of the meeting, accessed by ThePrint, it was discussed that while both allopathic medicine and AYUSH systems have been mainstreamed through Ayushman Bharat, there is a need to examine their integration in the Indian context.
A committee headed by Paul has been formed to propose a framework for the Integrative Health System, in order to achieve “inclusive, affordable, evidence-based, person-centric healthcare”. The committee will also develop a roadmap for disease prevention and health promotion in national programmes.
‘One Nation, One Health System’ has already been envisioned in the National Health Policy and the National Education Policy brought in by the Modi government in 2017 and 2020 respectively.
The NHP “recognises the need for integrated courses for ISM (Indian systems of medicine), modern science and Ayurgenomics (a combination of Ayurveda with the study of all the genes of an organism, called genomics)”. It also talks about getting AYUSH systems to contribute to “meeting the national health goals and objectives through integrative practices”.
As reported by ThePrint, the NEP states: “Given that people exercise pluralistic choices in healthcare, our healthcare education system must be integrative meaning thereby that all students of allopathic medical education must have a basic understanding of AYUSH and vice versa.”
Working groups to be made
While the ‘One Nation, One Health System’ policy is expected to be rolled out by 2030, four working groups will be made now in the core areas of education, research, clinical practice, and public health and administration.
These groups would study how countries all over the world — particularly the USA, China and European nations — have translated integrative medicine into their health system.
The groups will also study India’s own experience of integration of AYUSH and modern medicine, and also the legal aspects in the implementation of integrative medicine.
Implementing an integrative system would mean there will be a need for health professionals trained in such a system, according to a presentation shared at the 8 September meeting. So, the committee headed by Paul will also examine reforms in nursing education and regulation.
This report has been updated to include the health ministry’s response.
This report was first published in ‘The Print’ on September 25, 2020 here.